
Two nurses speak outside ORAU’s Medical Division
When ORAU was first established in 1946, the federal government contracted us to advise them on acquiring scientific personnel and to liaise with educational institutions and Clinton Engineer Works (the Oak Ridge production unit of the Manhattan Project, which would later become Oak Ridge National Laboratory). With 14 founding universities, we were very successful at accomplishing this goal. But, perhaps, what we’re most known for during our early years is our Medical Division. The Atomic Energy Commission (AEC—predecessor to the U.S. Department of Energy) had been looking into peacetime purposes for the nuclear science generated during WWII and commissioned three hospitals to explore the use of radioisotopes for cancer treatment: one near Argonne National Laboratory in Chicago, one near Brookhaven National Laboratory in Upton, New York, and one at ORAU in Oak Ridge.
In the 24 years of operation, the Medical Division of ORAU advanced nuclear medicine and cancer treatment in several tangible ways. Though this is not an exhaustive list, it includes the highlights from a couple dozen years of research and practice.
Here are seven gifts the ORAU Medical Division gave the world:
1. Advanced thyroid cancer understanding and treatment
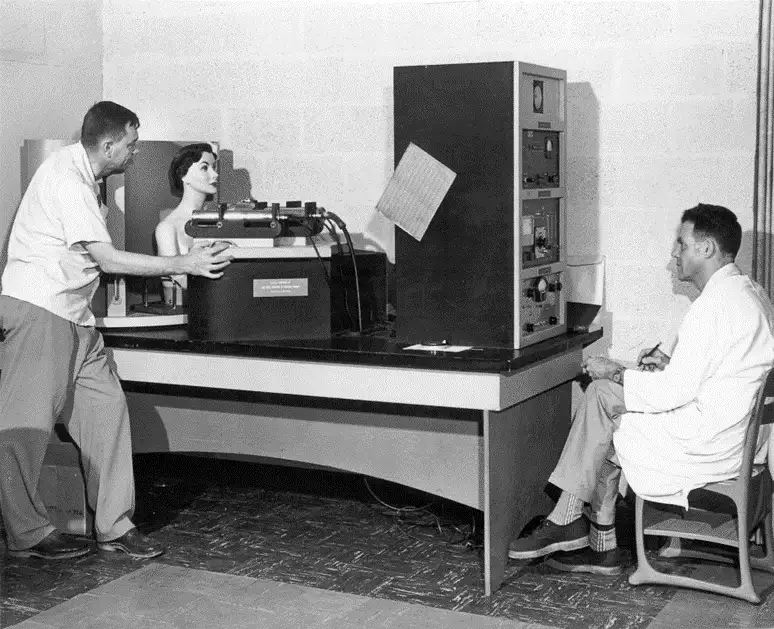
Dr. Brucer (left) testing one of his scanning manikins
ORAU contributed greatly to the treatment of thyroid cancer and diseases. Why the special interest in the thyroid? Remember, ORAU’s roots are in nuclear studies, and the thyroid gland is particularly susceptible to damage from radiation exposure because it absorbs and concentrates iodine, which is a common radioactive isotope released in nuclear accidents or incidents. Marshall Brucer, M.D., the first director of the ORAU Medical Division, was granted a patent for mock iodine. In the 1950s, iodine-131 was widely used to evaluate thyroid function, but it has an extremely short half-life, meaning it was not suitable for routine equipment calibrations for instruments used to measure iodine uptake (absorption). The mock iodine had a much longer shelf life and was helpful for medical staff to calibrate their counting machines before they were used on patients.
Not only did Brucer offer mock iodine, but he also created thyroid phantoms that simulated the human neck and thyroid. These “manikins” simulated the internal distribution of radiation within the human body and could be customized to mimic different body types and sizes. It was groundbreaking and used extensively for a few decades.
2. Whole-body radiation treatment
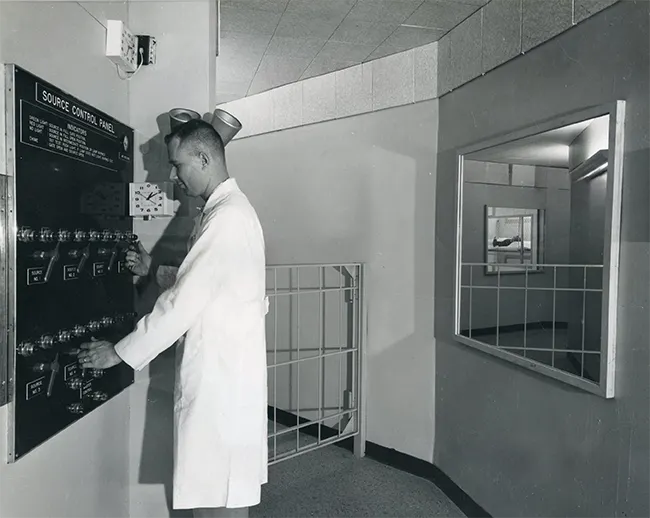
Medical Division staff provided whole body radiation treatments for patients who elected to receive them.
Until the 1960s, radiation instruments used to treat cancer did not provide uniform radiation fields. ORAU addressed this problem by designing and constructing a room to hold eight radiation sources that delivered a fixed dose at a moderate rate (METBI, the Medium Exposure Total Body Irradiator) in 1960. In 1967, the Low Exposure Total Body Irradiator (LETBI) was built. Between 1960 and 1974, about 200 cancer patients agreed to receive experimental treatment administered through these tools—often seeing it as a last-hope option in the fight against their disease.
The results of these treatments proved to be one of the biggest advancements in cancer research during this period and positioned ORAU as a pioneer in the emerging field of nuclear medicine. In fact, many people were able to extend their lifespans because of these treatments. Employing whole body irradiation (with significantly higher doses than those used at ORAU’s Medical Division) became the established medical practice for treatment of leukemia and other cancers.
3. Safer and more successful bone marrow transplants

Two marmosets living in ORAU’s research colony
ORAU chief scientist Nazareth Gengozian blazed a new trail when he established a colony of South American marmosets for his research in 1961. One set of studies showed that animals successfully transplanted with marrow genetically different from their own continued to have an impaired immune system. This indicated a critical need for finding the right donors for compatibility. Building on all that they were learning, ORAU’s Medical Division established a cytogenetics laboratory in 1964, and it became a major resource in providing a reliable technique for assessing human total-body radiation injury and chromosome analysis. Primarily, the cytogenetics lab was created to support research on the genetic effects of radiation exposure, providing chromosome analysis services for people who had been exposed to ionizing radiation (like people who worked in the nuclear industry or patients who had undergone radiation therapy). Even though finding the right donors for bone marrow transplants wasn’t the main purpose of the lab, this capability changed the game and greatly improved the success rate of marrow transplantation.
Dr. Gengozian also discovered that radiation delivered over a period of a few minutes was more effective for immunosuppression than the same amount of radiation delivered over the course of an hour. Thus, he developed the immunological basis for bone marrow grafting as we do it today. Previously, doctors attempted bone marrow grafting on very sick patients who were immunosuppressed and defenseless against infection. It was their last resort. They wanted to exhaust conventional wisdom of the time before trying a marrow graft.
Now, physicians know to bring in patients not handicapped by infection for this procedure. Dr. Gengozian’s sequence was to give the patient seven days of immunoglobulin, followed by total-body irradiation and within a few hours of the irradiation, Gengozian would do the bone marrow graft at a higher dose rate for a shorter amount of time. This led to one of the first successful bone marrow transplants for a leukemia patient.
4. New imaging options (whole-body scanners)
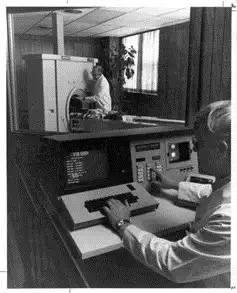
ECAT demonstration at ORAU
When Karl Hubner, M.D., made the move to the states from Germany to work in ORAU’s Medical Division, he thought he was ultimately going to be a pediatric hematologist and oncologist. After all, the reason he wanted to be in Oak Ridge was to do bone marrow transplants, but now, he was also intrigued by the detection of soft tissue tumors with X-rays and radiotracers. So, he started leaning more into imaging, and that became his passion. While at ORAU, his team developed whole-body scanners (teletherapy machines that focused beams of radiation on diseased tissue) and the Emission Computerized Axial Tomography (ECAT). This machine was a precursor to modern-day Positive Emission Tomography (PET) scanners. Today, PET scanners help doctors see the big picture—how well certain parts of the body are working. Physicians can tell how far cancer has spread and how well the patient is responding to treatment. This kind of information improves the success rate of treatment plans.
ORAU was the first organization to develop Gallium-67 as a scanning agent for locating soft tissue tumors. Gallium-67 still has wide use in nuclear medicine to this day.
5. Development of the Medical Internal Radiation Dose

Candid photo of Roger Cloutier
The 1960s was the right time to be in radiation research. The nuclear medicine field was growing, and new radioactive materials were being used in patient treatment plans. The ORAU Medical Division led the way in teaching medical professionals and emergency responders how to deal with radiation. As they taught physicians how to do dosimetry (that is, the science behind determining radiation dose by measurement and/or calculation), the Atomic Energy Commission and the Food and Drug Administration took notice and asked them to set up an internal dose information center, so doctors across the country would know how to administer the best care.
So, through the Society of Nuclear Medicine, ORAU employees Roger Cloutier and Evelyn Watson started the Medical Internal Radiation Dose (MIRD) to help physicians get answers about dosimetry. Cloutier became the chairman of MIRD. Meanwhile, the program Cloutier and Watson built at ORAU was officially established as the Radiation Internal Dose Information Center (RIDIC). The MIRD Committee still develops standard methods, models, assumptions and mathematical schema for assessing internal radiation doses from administered radiopharmaceuticals. The MIRD approach systematically reduces complex dosimetric analyses to methods that are relatively simple to use, including software tools.
6. New awareness of fetal dosimetry for pregnant women
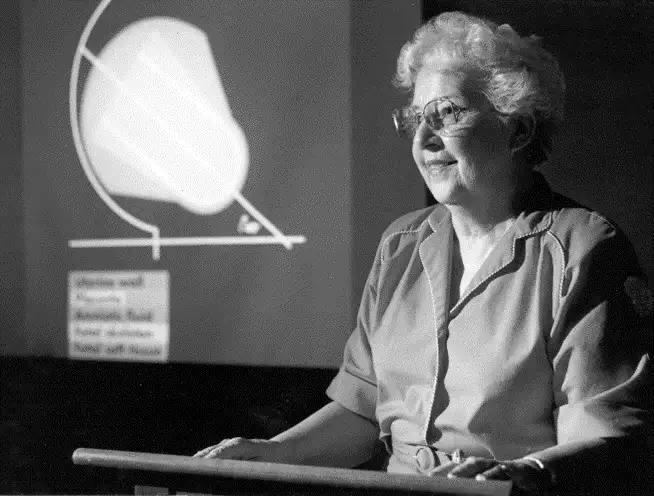
Evelyn Watson was a self-taught nuclear physicist who worked her way up the ladder at ORAU from a records clerk to the director of the Radiation Internal Dose Information Center. Watson was a mother, and as she learned what radiation exposure does to the body, she naturally wanted to learn more about the dangers of radiation exposure in women who are pregnant. Those in the field of fetal dosimetry credit Watson’s interest for major contributions. Not many people studied this area until she began looking into it. She served on the National Council on Radiation Protection and Measurements subcommittee on “Placental Transfer of Radionuclides” and on the editorial board of The Journal of Nuclear Medicine and as a consultant to the U.S. Food and Drug Administration Radiopharmaceutical Advisory Committee where she raised awareness to protect unborn children from radiation exposure. Learn more about Evelyn Watson’s contributions to the field of nuclear physics in this blog.
7. Creation of Radiation Emergency Assistance Center/Training Site

Photo from REAC/TS training exercise
With everything the staff at ORAU’s Medical Division learned, they petitioned the U.S. Department of Energy (DOE) for funding and approval to establish the Radiation Emergency Assistance Center/Training Site in 1976 as a radiation accident management facility for emergency treatment and acute patient care in the event of a major radiation exposure. Now part of the Oak Ridge Institute for Science and Education (ORISE, which is managed by ORAU for DOE), REAC/TS is a DOE asset funded by the National Nuclear Security Administration that provides 24/7 response and subject matter expertise on the medical management of radiation incidents. Through courses that include lectures and hands-on drills, REAC/TS is the domestic and international leader in nuclear disaster preparedness and training. To give you an idea of scope, in fiscal year 2023, REAC/TS hosted six on-site courses, two virtual webinars, 12 off-site trainings and five international courses for a total of nearly 1,000 highly specialized health care and response professionals instructed in radiation emergency response. And, keep in mind that REAC/TS has been around for 48 years! Part of what this team explores is cytogenetic biodosimetry (a proven technique that can be used to help calculate the absorbed radiation dose in people who are exposed to radiation—especially helpful following mass casualty incidents). Today, REAC/TS’ Cytogenetic Biodosimetry Lab is the only Clinical Laboratory Improvement Amendments-certified actively operational lab in the United States performing retrospective cytogenetic biodosimetry dose assessment.
So, what happened to ORAU’s Medical Division? By the early 1970s, the field of nuclear medicine had begun to really mature and many private hospitals around the country were offering their own high-quality nuclear medicine facilities. Thus, the mission the AEC set before ORAU was accomplished. Then, when budget deficits and inflation hit, the government decided to close the three AEC hospitals in 1974. ORAU continued treating patients on an outpatient basis and shifted its Medical Division focus to REAC/TS in 1975. What the world learned in the 24-year operation of ORAU’s Medical Division is still being applied toward nuclear medicine today.